METS program with funding PEPFAR/Centres for Disease Control (CDC) has supported the Ministry of Health/CPHL to scale up viral load (VL) monitoring to over 80% of the PLHIVs on ART between 2016 and 2017 with the use of a VL dashboard, support for curriculum development, capacity building trainings, and continuous quality improvement initiatives.
Introduction:
WHO recommends viral load testing as the gold standard for monitoring the response to ARV drugs, and a more sensitive and early indicator of treatment failure. In 2014, UNAIDS set the ambitious 90-90-90 targets to attain epidemic control by 2020 by the three pronged 90-90-90 approach thus:
- By 2020, 90% of all people living with HIV will know their HIV status.
- By 2020, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy.
- By 2020, 90% of all people receiving antiretroviral therapy will have viral suppression.
Up until August 2014, the mainstay of antiretroviral monitoring in Uganda was immunological testing using CD4 counts as well as clinical monitoring. With support from the Presidents Emergency Plan for AIDS Relief(PEPFAR), Uganda was selected as one of the countries in Sub-Saharan Africa to scale up virologically monitoring countrywide and the Ministry of Health through CPHL established mechanisms for scaling up viral load monitoring by tackling the possible bottlenecks to viral load scale up. These mechanisms were built on already existing systems for EID testing. They included: Centralised viral load testing at CPHL accredited lab, a robust sample transport and results return network, information systems, capacity building and logistics management among others.
METS support to the Country VL Monitoring approaches:
METS with funding from CDC has been very instrumental in the implementation of viral load monitoring countrywide. METS supported the following key activities:
- Demand creation for Viral Load services: METS works with CPHL and partners to create demand for viral load testing among PLHIVs and the public at large. We were involved in viral load campaign activities in February, July and August 2017. We developed a change package and communication materials for the campaign in collaboration with MoH, USAID/CHC and PEPFAR teams. We also host monthly viral load meetings that bring together development and implementing partners, district and health facility teams to deliberate on progress towards scale up targets and devise strategies and priorities for the viral load agenda.
- Development and revision of the viral load implementation and training manual. We have provided technical and financial support in the process of developing and revising the implementation and training manuals, job aides and standard operating procedures.
- Capacity building of health workers. METS has supported trainings and mentorships at District, Regional and Health Facility levels reaching over 1500 accredited ART sites within a one year period.
- Viral load data management and reporting at national and sub-national levels: METS has fully supported the functionalisation and utilisation of the viral load dashboard for data-driven decision making. We have also optimised the viral load dashboard to accommodate electronic results delivery in a bid to reduce results turnaround time. Additionally, we have supported the development and pilot of viral load tools and eventual integration into the national DHIS2. We have gone ahead to automate viral load monitoring tools into the UgandaEMR version 2.0
- Institutionalise application of quality improvement methodologies into routine services: METS in collaboration with Ministry of Health and district health teams has taken lead implementing a viral load Quality Improvement Collaborative in over 9 districts to address service gaps that were identified in 2015. We shall; document best practices to scale up countrywide.
National outcomes:
1.Increased number of PLHIVs accessing viral load testing services
The program has registered improvements across board. Annual sample volumes referred for viral load testing have increased five fold from 163,800 samples in COP14 to over 850,000 samples in COP16. The number of health facilities referring samples have also doubled from 835 in COP14 to over 1700 health facilities in COP16.
 This tremendous improvement has in turn had ripple effects at the district and national level. District viral load coverage is now over 90% in 58 districts and above 70% in 97 districts. Plans are under way to mount viral load campaigns in the northern and north-eastern districts to bridge the gap. By the end of COP16, over 70% PLHIVS on ART had a suppressed viral load test. This confers some significant protection against transmission of new infections at the population level and is commendable progress towards attainment of the third 90 for elimination of AIDS.
This tremendous improvement has in turn had ripple effects at the district and national level. District viral load coverage is now over 90% in 58 districts and above 70% in 97 districts. Plans are under way to mount viral load campaigns in the northern and north-eastern districts to bridge the gap. By the end of COP16, over 70% PLHIVS on ART had a suppressed viral load test. This confers some significant protection against transmission of new infections at the population level and is commendable progress towards attainment of the third 90 for elimination of AIDS.
-
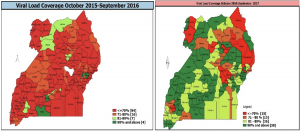
The maps below show the improvements country wide
Enhanced healthcare service Provider Skills:
Clinical and laboratory teams in over 1700 sites received training in viral load monitoring including sample collection, logistics management, routine and intensive adherence counselling, results interpretation, CQI and monitoring and evaluation.
- Improved documentation and data management and reporting for viral load services
METS organised national trainings and pilot of viral load monitoring tools in over 64 health facilities across the country. We worked with MOH and partners to develop and review materials including the non-suppressed register and viral load addendum 113 to the HIV Quarterly report 106a. The successful pilot has led to a lot of demand from stakeholders to scale up the pilot tools to all ART accredited sites to augment the viral load dashboard. METS has and continues to support development and upgrade of the national viral load dashboard to optimise it for reporting, results delivery and monitoring of program performance.
Improved stewardship by MOH to deliver quality viral load services. METS works with MOH and PEPFAR teams to embrace delivery of quality management systems at all levels through: stakeholder meetings, data review and feedback sessions, and continuous quality improvement initiatives. This ensures that viral load activities are tracked and discussed with implementing partners, DHTs and health facility teams for improved program outcomes.
Next steps for METS
Despite the enumerated achievements above, we still have gaps that need to be bridged in the immediate term. The recent UPHIA results showed a grim picture for population level viral suppression rates at 59.7% among adults 15-64 years and 39.2 % among children less than 15 years. Children, adolescents and men were also disproportionately affected by poor suppression rates. METS will work with development and implementing partners to prioritise the affected populations using available structures such as OVC services and family support groups.
METS will also prioritise scale up of viral load monitoring tools in the national HMIS structure in the new program year.
HIV Drug Resistance Testing has started for clients failing on second line. METS is working with CPHL and the HIVDR testing labs-JCRC and UVRI to extend services to clients failing and provide results to the third line sub-committee to make informed decisions in selecting third line treatment options.
METS will also work with MOH and implementing partners to improve viral load results utilisation for better and timely management of non-suppressed clients on ART.
Uganda is on track to achieving the UNAIDS 90-90-90 targets and provides a good model in sub-saharan Africa for transitioning from immunological to virologic monitoring of clients on ART.
Article by Dr. Miriam Murungi,Program Officer-CBS